The 1st VHIO-BBVA Foundation International Symposium on Cell-based Therapies in Oncology , organised by Dr. Alena Gros, head of the VHIO Tumour Immunotherapy & Immunology Group, and Dr. Sonia Guedan, leader of the IDIBAPS Cellular Immunotherapies for Cancer Research Group, is due to be held on 29 and 30 November. The aim of this meeting, sponsored by the BBVA Foundation through the Comprehensive Cancer Immunotherapy and Immunology Program (CAIMI and CAIMI II), is to disseminate the results of high-quality research in the field of advanced therapies and to foster collaboration among international experts to advance our understanding of cancer and ensure research results reach clinical practice to the benefit of cancer patients.
Over recent decades, the emergence of immunotherapy has led to a paradigm shift in cancer treatment and enormous benefits for patients. “However, despite the promising anti-tumour responses, currently only some patients treated with immune checkpoint inhibitor therapies respond, while some also experience autoimmunity-related adverse events. Thus, there is a clinical need to personalise and develop new immunotherapies”, explained Dr. Alena Gros, head of the VHIO Tumour Immunotherapy & Immunology Group.
Development of advanced therapies in cancer
Advanced therapies are based on the use of genes, cells and tissues, both genetically modified and unmodified, and are considered permanent or long-term therapeutic solutions for acute or chronic human diseases. According to the Spanish Association of Biotechnology Companies (ASEBIO), in 2020 there were over a thousand active clinical trials involving advanced therapies worldwide, most of them (62%) in the field of oncology.
“In the case of cancer, advanced therapies aim to redirect the patient’s immune system specifically against tumour cells to effectively eliminate them, thus strengthening the patient’s defences against the tumour”, said Dr. Gros.
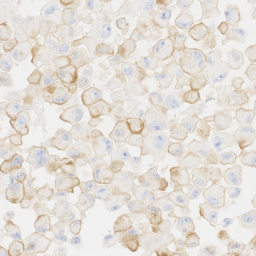
Currently, the most frequently used strategies to achieve this are therapies with TILS and CAR-T cells. But how do they work? In the case of therapies with TILs (tumour-infiltrating lymphocytes), immune cells containing lymphocytes capable of recognising and attacking tumour cells are extracted from the patient’s tumour. These are activated and expanded in the laboratory and then infused back into the patient to act more effectively against the tumour cells. CAR (chimeric antigen receptor) T-cell therapy is based on genetically modifying lymphocyte populations so they specifically recognise and attack tumour cells.
“Advanced therapies in oncology, especially with TILs, CAR T-cells and natural killer cells, among others, are an opportunity to make a qualitative leap forward in developing new, truly personalised therapeutic strategies to offer to cancer patients who do not respond to other treatments”, stated Dr. Joaquin Arribas, head of the VHIO Growth Factors Group, which is working to develop new CAR T-cell therapies for breast cancer.
A consolidated programme
In recent years, the VHIO has set up a multidisciplinary working team with enormous experience in clinical, preclinical and therapeutic product development research with the support of the BBVA Foundation through the Comprehensive Cancer Immunotherapy and Immunology Program (CAIMI and CAIMI II). As part of this program, various VHIO groups, such as those of Dr. Alena Gros and Dr. Joaquin Arribas, are researching the development of new products such as TILs, natural killer cells and CAR T-cells, among others.
The concession in 2022 of the Spanish Association Against Cancer’s AECC Excellence Program – Advanced Therapy Accelerator will enable the VHIO Advanced Therapies Program to take a leap forward by building a clean room, a laboratory that meets the necessary quality and health safety standards to manufacture cell therapy products for clinical use in the European Union.
“This new infrastructure will enable us to generate new products developed in VHIO under highly controlled environmental parameters and increase the options for cell therapies produced in our centre”, stated Dr. Martín-Lluesma, director of the VHIO Advanced Therapies Program. “But above all, it will allow us to develop new products and test them in earlier phases, prioritising those we believe could be more beneficial to our patients”.
Developing these products requires the right teams, equipment, technology and experience and, in this sense, thanks to the VHIO Research Unit for Molecular Therapy of Cancer, the UITM-CaixaResearch, headed by Dr. Elena Garralda, nine clinical trials for cell therapies in solid tumours are been conducted, five of them in early stages. “Our end goal is to get these new cell products sustainably into the service portfolios of the national health systems, so that all patients have access to these types of therapy if they need them”, said Dr. Garralda.
For his part, Dr. Pere Barba, researcher with the VHIO Experimental Hematology Group and director of the Vall d’Hebron University Hospital Haematology Department Advanced Therapies Unit, explained that “currently in the Unit we have 21 active clinical trials for new cell therapies for haematological and cancerous neoplasia and autoimmune diseases, most of them with CAR T-cells”.
Model of translational research.
The VHIO Advanced Therapies Program is part of the translational research model which characterises the institution, in which research results are effectively and safely transferred to clinical practice through clinical trials. The model has led to the VHIO becoming the first research institute associated with a healthcare centre to be accredited as a Severo Ochoa Centre of Excellence for its experience and leadership in clinical trials, especially in early phases and with experimental drugs, and for its translational research model involving close coordination between preclinical and clinical research.