- Recently published open access in the Journal for ImmunoTherapy of Cancer (1), findings from a study led by VHIO’s Alena Gros advance insights into the underlying biology of tumor-reactive T cells in endometrial cancer (EC).
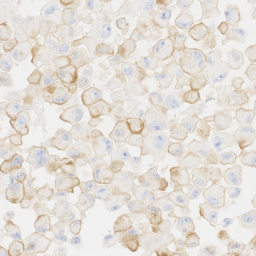
- The investigators report a combination of biomarkers capable of distinguishing the CD4+ and CD8+ tumor-reactive lymphocytes from other T cells present in human tumors. The presence of these markers in the tumor microenvironment correlates with improved survival in EC patients.
- The described biomarkers show promise in predicting prognosis in EC patients undergoing surgery, and could be used to select, enrich, and multiply these T cell subsets as cell-based immune therapy.
Endometrial cancer (EC) is the sixth most commonly diagnosed cancer in women, with 417,000 new cases and 97,000 deaths in 2020 (2). Immunotherapy is an emerging area of research and treatment for EC either as monotherapy or in combination with other targeted agents.
While immune-based treatments are increasingly stepping up in improving outcomes in this patient population, advancing insights into the prevalence, phenotype, specificity, and prognostic value of tumor infiltrating lymphocytes (TILs) is required to identify robust biomarkers of response that could better guide treatment decision making.
TILs are T cells that recognize cancer cells and penetrate into the tumor. Tumor-reactive lymphocytes can kill cancer cells although in many cases the antitumoral immune response is deactivated. To better understand the role of TILs in EC, researchers led by Alena Gros, Principal Investigator of the Vall d’Hebron Institute of Oncology’s (VHIO) Tumor Immunology and Immunotherapy Group, analyzed EC resident T cells from 47 primary tumors.
“We aimed to identify subpopulations of tumor-reactive CD8+ and CD4+ TILs that could be exploited to develop personalized T-cell based therapies. In our search for this, we found that these were also prognostic and predictive biomarkers of prolonged survival in endometrial cancer,” says Alena Gros, corresponding author of this present study.
Recently published open access in the Journal for ImmunoTherapy of Cancer (1), data show that the majority of tumor-reactive CD8+ TILs co-express PD-1 and CD39, as well as CXCL13. Further, CD4+ TILs that express high levels of PD-1 as well as CXC13 also exert an immune response against tumors, independently of CD39 expression. In both cases, CD8+ and CD4+ TILs associate with improved survival in patients with endometrial cancer.
The authors report that CD4+ and CD8+ TILs that recognize and kill cancer cells are characterized by expression of PD-1, CD39 and CXCL13 in CD8+ cells; and expression of CXCL13 and high levels of PD-1 in CD4+ cells.
“These markers could be used to develop more effective and personalized adoptive cell therapies where populations of tumor-reactive CD4+ and CD8+ TILs can be selected, enriched, and multiplied in the laboratory, and subsequently readministered to the patient to induce an anticancer immune response.” explains Gros.
Results suggest that the characterization of tumor-reactive TIL subsets could advance insights into disease evolution and help to predict response to therapy. The researchers analyzed TIL populations in primary tumors of patients that had undergone surgery. The presence of these specific subpopulations of tumor-reactive T cell populations could ultimately help guide treatment decision making. For example, patients without these subpopulations could receive a more intensive treatment with adjuvant therapy after surgery to attempt to delay cancer regrowth.
“Our data provide deeper insights into the biology of tumor-reactive T cells that infiltrate EC as well as a new approach to distinguish between these and other CD8+ and CD4+ cells that are found in the tumor but do not assume such an important a role,” adds Jara Palomero, a Postdoctoral Fellow of Alena Gros’ group and first author of this study.
“Given that the immune system and the expression of the described biomarkers behave in a similar way, independently of the tumor type, these markers could also be useful in patients with other types of cancer,” concludes Gros.
This research was funded by support received from the BBVA Foundation’s Comprehensive Program of Cancer Immunotherapy and Immunology (CAIMI), the TV3 Fundació La Marató, Spanish Ministry of Science and Innovation, Carlos III Health Institute, CERCA Research Centres of Catalonia, Beatriu de Pinós research programme, Agency for Management of University and Research Grants (AGAUR), and the HORIZON 2020 EU Framework Programme or Research and Innovation.
###
References:
- Palomero J, Panisello C, Lozano-Rabella M, Tirtakasuma R, Díaz-Gómez J, Grases D, Pasamar H, Arregui L, Dorca Duch E, Guerra Fernández E, Vivancos A, de Andrea CE, Melero I, Ponce J, Vidal A, Piulats JM, Matias-Guiu X, Gros A. Biomarkers of tumor-reactive CD4+and CD8+ TILs associate with improved prognosis in endometrial cancer. J Immunother Cancer. 2022 Dec;10(12):e005443.
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021 May;71(3):209-249.